Dementia is a multifaceted condition that affects millions of individuals worldwide, with varying symptoms that progress over time. Recognizing the progression of symptoms is valuable for patients, caregivers, and medical professionals. By understanding the stages of dementia, we can provide support and interventions. In this article, we will explore the signs and symptoms at each stage and offer insights into managing the challenges that arise.
Table of Contents
Early Signs of Dementia and How They Progress
The initial symptoms of dementia can be subtle and often mistaken for normal aging. Individuals may experience memory lapses, difficulty finding words, or lose track of the date and time. Personalities may begin to change, and social withdrawal can occur as tasks and engagements become more challenging. These early signs are crucial in recognizing the onset of dementia and prompt a closer evaluation. Over time, these symptoms can manifest into more noticeable cognitive impairments.
As these early symptoms progress, establishing a support network is critical. Family members should become acquainted with the dementia stages, enabling them to provide better care. Initiating legal and financial planning during this time can also alleviate future stressors as the person’s ability to manage complex tasks diminishes. Problems with short-term memory advance, and performing familiar tasks becomes more cumbersome.
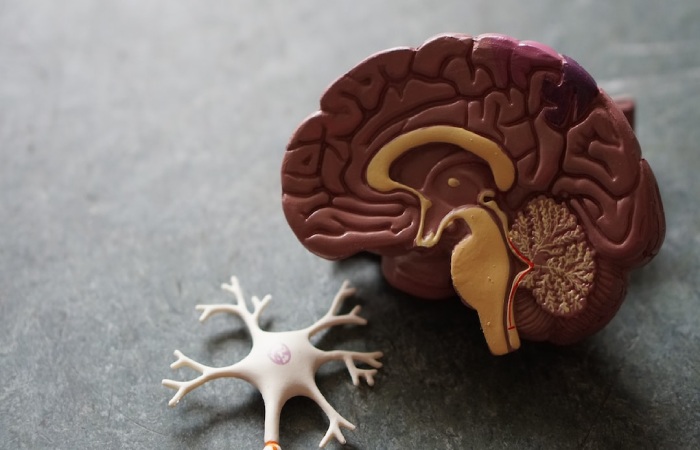
This stage can be confusing for individuals as they are often aware of their declining abilities, creating frustration and anxiety. You have to ensure empathy and support during this period. Discussing concerns with a healthcare provider can lead to early intervention, which may slow the cognitive decline. Diagnostic evaluations will consider the individual’s medical history, cognitive testing, and possibly brain imaging. At this juncture, focusing on a healthy lifestyle and possibly pharmacological intervention is necessary.
Understanding Mild Cognitive Impairment (MCI)
Mild Cognitive Impairment is a stage between the expected cognitive decline of normal aging and the more severe decline characteristic of dementia. Individuals at this stage may experience noticeable lapses in cognitive functions, such as memory, thinking skills, or judgment, which do not yet hinder daily activities. Distinguishing MCI from the early stage of dementia can be challenging but is required for outlining appropriate care strategies.
Not all MCI cases progress to dementia, so ongoing assessment is vital. Cognitive training and medication may be able to manage symptoms or potentially slow progression. Lifestyle modifications can play a pivotal role in managing MCI. Consistent social engagement, regular physical exercise, and a heart-healthy diet could have positive effects on cognitive health. Emphasizing these activities can help maintain an individual’s quality of life and independence for as long as possible.
Navigating Moderate Dementia and Lifestyle Adjustments

During moderate dementia, the challenges become more pronounced. Individuals may struggle with routine activities, like dressing or bathing, and need assistance. Recognizing faces and understanding environmental cues often decline, which can result in disorientation, even in familiar settings.
Personality and behavioral changes often surface during moderate dementia. Patients might exhibit increased restlessness, suspicion, depression, or even aggressive episodes. Coping with these changes demands patience and a structured routine from caregivers to provide a sense of stability and safety.
At this stage, home safety becomes a priority. Adjusting living spaces to reduce risks, like falls, and simplifying navigation can significantly impact the individual’s well-being. Professional caregiving services may be introduced to support the family and guarantee proper care. Despite the increasing need for supervision, it’s essential to encourage independence where feasible. This holistic approach supports the individual’s dignity and quality of life.
Late-stage Dementia: Recognizing End-of-Life Symptoms
In the final stage of dementia, cognitive function continues to decline, leading to near-total dependence on care. Individuals may become bedridden, and their ability to communicate may be limited to non-verbal sounds. During this time, the focus of care is on comfort and preserving human dignity. Recognizing and managing end-of-life symptoms is paramount in late-stage dementia care. Signs such as reduced appetite, changes in breathing patterns, and decreased responsiveness need sensitive management.
Decisions regarding medical interventions and advanced directives should align with the known or inferred wishes of the individual. These are delicate discussions that families must engage in with healthcare professionals to be sure that care is compassionate and appropriate. Families may also seek the support of hospice services, which specialize in end-of-life care. This provides the individual with specialized attention and offers emotional support to family members during a challenging period.
As you can see, understanding the progression of dementia and adapting care accordingly can profoundly influence the lives of those affected. Engaging with professionals, accessing resources for support, and prioritizing the quality of life at each stage can help individuals and their loved ones navigate the complexities of this condition with dignity and compassion.

